Stomatitis: What Is It, Causes, Signs, And More
Published January 2, 2024
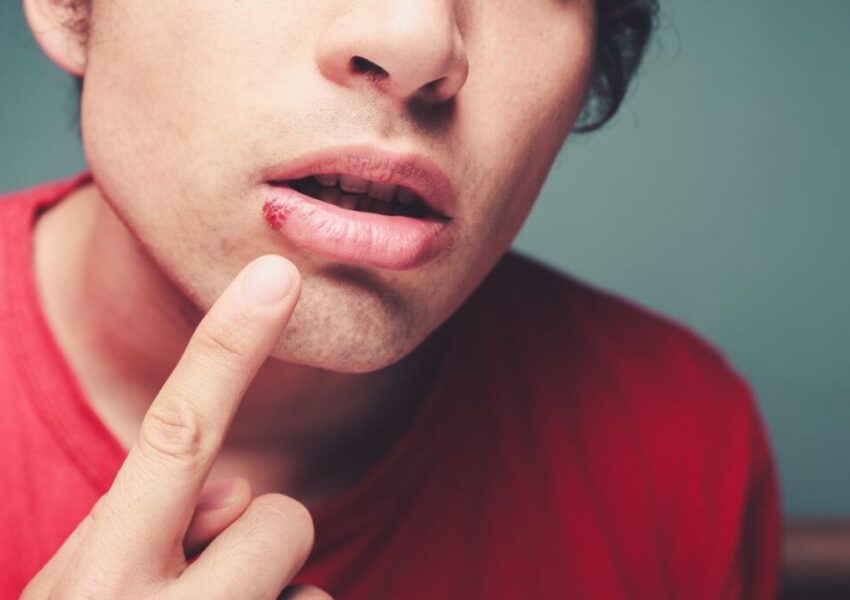
Picture a scenario where basic actions like eating, speaking, or smiling become excruciating tasks. Sadly, this is a harsh reality for individuals battling stomatitis. It’s a condition that involves inflammation of the mucous membrane within the oral cavity.
Stomatitis is more than oral discomfort. It disrupts daily life, interrupting routines and diminishing the quality of interactions. The condition has viral, bacterial, or fungal origins. It also has other contributing factors. These complexities emphasize the need for timely management.
In this article, we’ll explore the stomatitis causes, symptoms, diagnostics, treatments, and prevention. It’s time to navigate its challenges and regain control over your oral health and well-being.

What Is Stomatitis?
Stomatitis is defined by the inflammation and redness of the oral mucosa. The condition can affect the gums, tongue, inner cheeks and lips. It can bring about discomfort and difficulty eating, talking, and sleeping.
There are two main types of stomatitis—cold sores (herpetic) and canker sores (aphthous).
- Cold sores. They have small, painful sores filled with fluid. The sores form on or around the lips near the borders of the mouth. It’s brought about by the herpes simplex virus (HSV). The condition is also called herpes stomatitis. Cold sores can last for around 5-7 days and can continue to come back. Sadly, these sores are contagious.
- Canker sores. These are also called aphthous ulcers and the common cause of stomatitis. The sores are pale white or yellowish with a red outer ring, leading to acute, brief pain. Canker sores form individually or in a cluster, usually on the inside of the lips, cheek, or tongue.
Stomatitis can disrupt oral health, complicating hygiene practices. The discomfort associated with the condition makes brushing and flossing challenging. If left to progress, the condition can worsen. It has the potential to cause complications. These include secondary infections or difficulty in eating and swallowing.

What Causes Stomatitis?
The stomatitis causes can vary significantly. The condition can be caused by viral or bacterial infections. In some cases, it can be due to autoimmune disorders or certain medications. Pinpointing the root causes is crucial to manage the situation effectively.
- Viral infections due to the herpes simplex virus (HSV)
- Common cold viruses such as Coxsackievirus (hand, foot, and mouth disease) or adenovirus
- Yeast infections, such as thrush
- Certain strains of Streptococcus bacteria, particularly Streptococcus mutans and Staphylococcus aureus
- Sexually transmitted infections
- Allergic reactions to specific foods, medications, or oral care products
- Nutritional imbalances particularly on vitamin B12, iron, or folic acid
- Irritants such as smoking or chewing tobacco
- Any form of trauma to the oral cavity. It can range from biting the interior of the cheek, lip, or tongue. It can also result from burning the mouth with hot food or drinks. In some cases, poorly-fitting dentures and surgery can cause the sores.
- Chemotherapy treatment for cancer
- Conditions associated with dry mouth

Stomatitis Symptoms
The condition often brings about discomfort, soreness, and stinging sensation. In every case, the symptoms vary and may include the following:
- Oral ulcers and lesions have a yellow or white layer and red base. Most usually form within the lips, cheeks, or on the tongue.
- Reddened or swollen patches
- Blisters
- Burning sensation in the mouth
- Fever and general malaise
Seeking immediate medical care is essential for an accurate diagnosis. Doing so ensures the proper treatment is started. This minimizes symptoms and prevents complications.
How Is Stomatitis Diagnosed?
A healthcare professional will examine the oral cavity. They’ll do this to identify the characteristic signs of stomatitis.
Other tests might include the following:
- Viral and bacterial swabs
- Tissue scraping or swabs for fungal infections
- Biopsy or removal of tissue or cells
- Patch tests to identify allergy
- Blood tests
The medical history of the individual will also be under scrutiny. The reason is to determine if a current or previous medication is responsible for stomatitis. Additionally, the doctor will also ask about sexual history and smoking habits.

Treatment For Stomatitis
The treatment for stomatitis will be based on the root cause.
- Medications and antivirals. If a virus is the root cause, the doctor will prescribe antiviral drugs. Examples include acyclovir or valacyclovir. These medications help manage viral replication. They also minimize the severity and duration of the outbreaks. Antibiotics such as penicillin or erythromycin will combat the infection. They’ll also reduce the symptoms if bacteria are responsible.
- Mouth rinses. Mouth rinses contain antimicrobial or anti-inflammatory agents, such as chlorhexidine or hydrogen peroxide. These work by reducing oral inflammation and preventing infection.
- Topical applications. Topical treatments, like corticosteroids or antifungal creams, are applied to the affected areas. They minimize pain, swelling, or fungal growth.
Treating the underlying factors contributing to stomatitis is vital for effective management. It involves dealing with nutritional deficiencies with dietary changes. As for allergies, it may include avoiding specific triggers. Additionally, quitting tobacco or minimizing oral trauma helps prevent recurrent episodes.
Preventive Measures
If you want to lower your risk of developing stomatitis, observe these basic precautions. For example:
- Maintain good oral hygiene with regular brushing with fluoride toothpaste and gentle flossing.
- Use an antiseptic and non-alcoholic mouthwash.
- Use a soft-bristled toothbrush to minimize potential trauma to your oral cavity.
- Avoid irritants such as tobacco products.
- Follow a well-balanced diet rich in essential vitamins (B vitamins). Aside from Vitamin B complex, you can also boost the immune system by including foods rich in antioxidants, zinc and vitamin C. Additionally, probiotics are also worth considering to help strengthen your immune system.
- Schedule routine dental check-ups

Be Proactive In Stomatitis Management
Stomatitis is characterized by inflammation and various uncomfortable symptoms in the oral cavity. It can disrupt daily life and well-being. Identifying and managing this condition is crucial to prevent a detrimental impact on quality of life. Timely intervention helps ease discomfort and prevents potential complications from arising.
Be in control of your oral health by being proactive. Know the stomatitis causes and act right away if you experience any of the symptoms. Focus on getting professional care to ensure good oral health.
Benefit From The Latest Advancements In Probiotic Science With Bionaze
Bionaze is a proprietary blend of probiotics proven to promote ear, nose, and throat health, improve digestion, and support your immune system. The active ingredients BLIS K12, and BL-04 are considered among the best probiotics according to science.
Get 25% Off Your First Order when you use BIO25 at checkout!

This Content Has Been Reviewed For Factual Accuracy
This content has undergone thorough fact-checking by our team of internal experts. Learn more about the meticulous editorial standard for our website here.
ADVERTISEMENT

About The Author
I am Tracy Gorman, a seasoned writer passionate about creating helpful content. I can delve into any niche and produce valuable articles with my expertise. Beyond writing, I am an avid learner with a passion for digital marketing. During my leisure time, I enjoy immersing myself in literature, experimenting with fashion, staying active, exploring culinary delights, indulging in movies, savoring music, and socializing. And, it’s safe to say, I love cats!